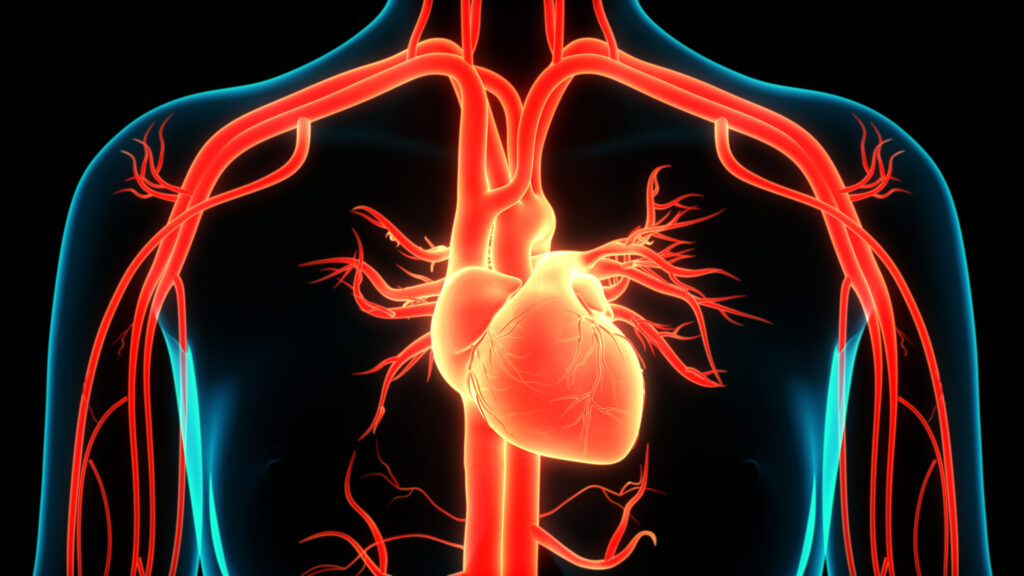
Anesthesia plays a crucial role in facilitating surgical procedures, ensuring the patient remains pain-free and the surgeon can work without hindrance. However, the impact of anesthetic drugs on the myocardium, the muscular layer of the heart, is an area of particular concern and interest among medical professionals. This is especially significant as the heart’s function determines the perfusion of tissues, including vital organs, during surgery. The effects of anesthetic agents on the myocardium range from changes in heart rate and rhythm to myocardial contractility and coronary blood flow.
Many general anesthetic agents, including volatile anesthetics like halothane, isoflurane, and sevoflurane, have been observed to cause a dose-dependent depression of myocardial contractility. This effect is mediated through the attenuation of calcium influx into myocardial cells, leading to reduced calcium availability for contraction. This decrease in contractility can result in reduced cardiac output, which can be particularly concerning in patients with compromised heart function.
Anesthetic drugs can influence the autonomic nervous system, thereby affecting heart rate and rhythm. For instance, halothane is known to sensitize the myocardium to catecholamines, increasing the risk of arrhythmias. Moreover, volatile anesthetics can produce a vagal predominance, leading to bradycardia. Conversely, ketamine, an NMDA receptor antagonist, may cause tachycardia due to its sympathetic stimulating properties.
The relationship between coronary blood flow and myocardial oxygen consumption is a delicate balance that can be altered by anesthetic drugs. While a reduction in myocardial contractility and cardiac output might theoretically decrease myocardial oxygen demand, some anesthetic agents can cause coronary vasodilation, thereby potentially increasing coronary blood flow. For instance, isoflurane is known to produce coronary vasodilation, which can help prevent coronary artery spasm during surgery. However, redistribution of coronary blood flow might result in areas of the myocardium receiving reduced oxygen supply, predisposing these areas to ischemia.
Emerging research suggests that some anesthetic agents, especially volatile anesthetics, might offer myocardial protection against ischemia-reperfusion injury. This phenomenon, termed anesthetic preconditioning, involves the activation of intracellular signaling pathways that can render the myocardium resistant to injury from subsequent ischemic episodes. Mechanisms underlying this protective effect include increased production of endogenous antioxidants and preservation of mitochondrial function.
While global myocardial depression can be seen with various anesthetic agents, some drugs can produce regional differences in myocardial function. This is particularly evident in patients with existing coronary artery disease. Areas of the myocardium supplied by stenosed or occluded coronary arteries might be more susceptible to the depressant effects of anesthetic agents, leading to regional wall motion abnormalities. Such regional dysfunction can compromise overall cardiac function and, in severe cases, may precipitate heart failure.
It’s vital to consider the interaction of anesthetic drugs with other medications that affect the myocardium. For instance, beta-blockers, commonly prescribed for hypertension and other cardiovascular conditions, can further depress myocardial function when combined with anesthetic agents. On the other hand, certain drugs like calcium channel blockers might mitigate some of the negative effects of anesthetics on the myocardium.
The effects of anesthetic drugs on the myocardium are multifaceted, with potential implications for patient care during surgery. Anesthesiologists must be acutely aware of these effects to tailor anesthesia delivery optimally. The choice of anesthetic agent, its dose, and administration method should be individualized based on the patient’s cardiovascular status and the surgical procedure’s specific demands. By understanding the intricate relationship between anesthetic drugs and the myocardium, medical professionals can ensure optimal cardiac function and patient safety during surgery.